Thymic Regeneration
Fighting the day everlasting
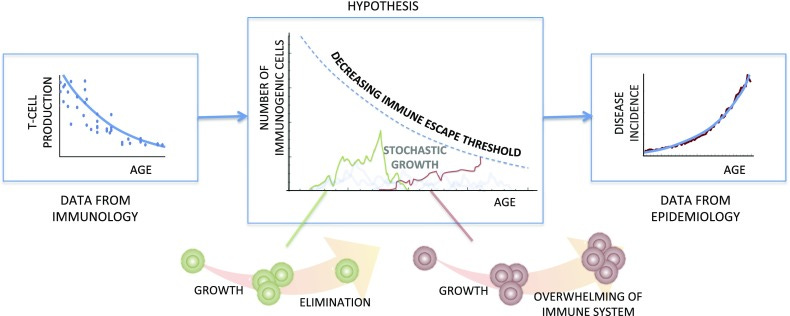
Moving from the heart of being to the being above the heart, if one were to want to improve the healthy lifespans of the world's (wealthier(1)) populations, a fascinating topic is whether we can slow down or reverse thymic involution. In humans, the thymus atrophies, in contrast to other organs, since infancy with an exponential decline in trained T cell production with a half-life of approximately 16 years. Gradual decline in thymus function has been found to strongly correlate with the incidence of a broad array of diseases, whether contagious or cancerous, as an apparent power law (Palmer et al. 2018). Would keeping the thymus fit, therefore, just by itself keep us much healthier in middle- and old age?
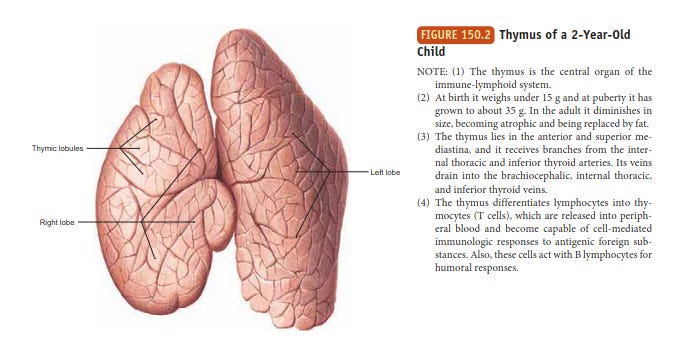
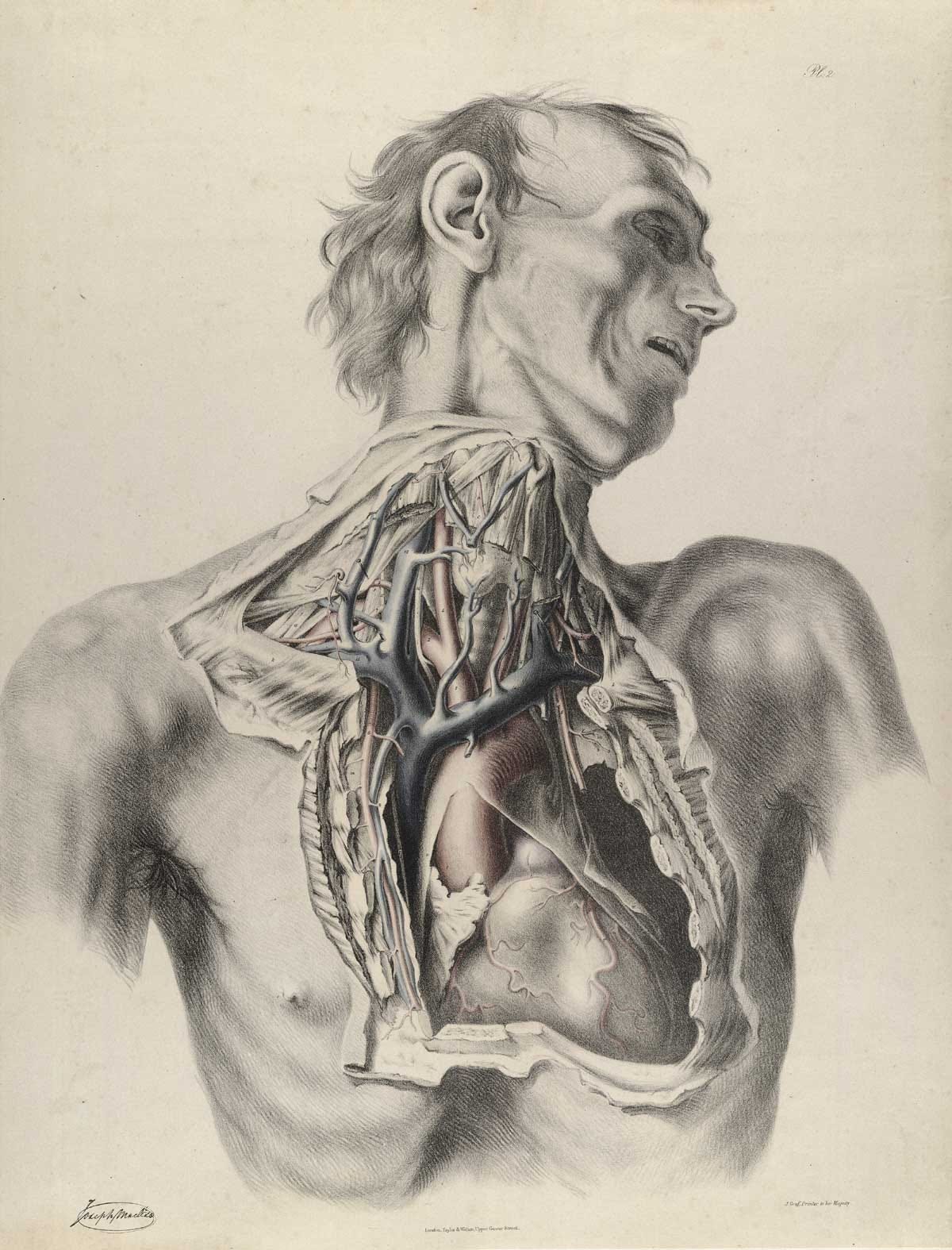
The thymus is where T cells (the T stands for thymus) coming from bone marrow undergo a rigorous selection process. Immature T cells are selected for their ability to interact with the body's own cells whilst not reacting too strongly to the body's own antigens. The cells surviving boot camp are then moved to the barracks to be trained to recognize specific antigens whilst taught how to be tolerant of the body's own tissues. So this little organ shaped like a dead butterfly turns out to be very essential to a well-functioning immune system.
Yet the thymus degenerates almost from the get-go. For an unknown reason, this process begins in infancy with a rate of about 3% decrease in function every year, slowing down in middle age. There may have been evolutionary pressure to maintain this feature, perhaps to allow for the redistribution of resources to other parts of the body in youth. If that is so, boosting the thymus in maturity could be done without worries about the role thymic degeneration might play in human developmental balance. Since a strong link between degraded thymic function and disease incidence seems to have been established in recent years, there's now greater research activity around thymus regeneration. How might we accomplish this?
Starting with the basics, castration (an often tempting solution to life's various problems) shows some promise regarding slowing down thymus degeneration, but based on mouse tests, the results are not terribly long-lasting.
Next, regenerative medicine. Various forms of research here are advancing rapidly in general, so can we hope to have transplants of entire thymuses or thymus tissue to address the problem? This is an active area of research across different approaches, such as bioengineered artificial tissues, cellular reprogramming, and gene therapy. Here, we might hope for early-stage clinical trials of thymus rejuvenation techniques in 5-10 years, first-generation treatments in 10-20 years, and fully functional artificial ultra-pro thymuses as well as personalised thymus rejuvenation therapies in 20-30 years.
For earlier results, we might look to growth factor hormones, such as interleukin-22, insulin growth factor 1, and thymosin. There's hope that a growth factor intervention could stimulate thymic epithelial cell production, enhance T cell production, halt or reverse involution, and/or help repair damaged thymic tissue. Limited application along these lines after clinical trials might be available within a decade. More outlandish options might include hibernation (some animals regenerate their thymuses during their hibernation), nanoparticle delivery, xenotransplantation from pigs or gut microbiome alteration.
A possible immediately available (though less revolutionary) remedy, however, is to live in natural darkness or devour heaps of melatonin. Melatonin, the natural hormone produced especially in response to darkness, has been shown to enhance the proliferation of T cells and help in the maturation of T cells in the thymus. Moreover, some further studies point to how melatonin can slow thymic involution. The typical over-the-counter melatonin dose is between 0.5 and 5mg, though I have met people who regularly consume up to 1g daily. What's a few orders of magnitude between friends? The long-term impacts of high-volume melatonin consumption are understudied, though no known overdose cases have been seen; it is not addictive, has a short half-life and has limited receptor activity due to saturation effects. Those long-term studies I've seen don't show significant negative effects.
The helpfulness of melatonin here (not to mention in a surprising amount of other places) raises questions about stealthy population-level health impacts that we might be facing from our modern life rhythms vastly modulated by artificial light. Melatonin is found in the mitochondria of various cell types in our body; it crosses cell membranes and the blood-brain barrier and is fairly ubiquitous. Artificial light, particularly on blue wavelengths, notoriously disrupts the natural cycle of melatonin production. Constantly disrupting the availability of a seemingly essential and largely omnipresent hormone doesn't feel like the wisest possible course of action, though of course, money never sleeps, and we must remain productive, or at least bathed in light, at all times apart from the minimal sleep hours we are granted.
Will we, in a decade or two, collectively awaken to treating light in darkness as we now treat cigarettes?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9381902/
https://rupress.org/.../Generation-and-repair-of-thymic...
Melatonin fanatics seem to congregate here:
https://www.facebook.com/doris.loh.23
(1) From our fortresses of paradise we sometimes forget that in all too many places getting to the advanced age of 40, where things like increased disease incidence due to thymic involution might even begin to be a worry, is a status symbol in itself. Dying of cancer? Congratulations! Happy you've made it this far in life, sir.